(April 10, 2011): Last week, it was announced that NCI, Inc., one of the nation’s most successful information technology companies had acquired the outstanding capital stock of AdvanceMed Corporation (AdvanceMed), an affiliate of CSC. While the acquisition went largely unnoticed by the health care provider community, the transaction may, in fact, be quite significant. With this acquisition by NCI, a recognized powerhouse in information technology, Medicare and Medicaid providers should expect AdvanceMed’s expertise in data mining and investigations to continue to grow. Medicare and Medicaid providers have an affirmative obligation to ensure that operations, coding and billing activities fully comply with applicable statutory and regulatory requirements. As NCI-owned AdvanceMed continues to fine-tune its data mining efforts and further expands its ability to conduct "Predictive Modeling," providers will likely find their actions under the microscope like never before. It is therefore imperative that all health care providers immediately implement an effective Compliance Plan (if they have not already done so) or further enhance their current compliance efforts. The purpose of this article is to briefly report on NCI-owned AdvanceMed and discuss the changes, if any, that Medicare providers and suppliers should expect. An overview of the current ZPIC environment is also provided.
I. Background of NCI's Acquisition of AdvanceMed:
NCI first announced its plans to acquire AdvanceMed last February. As NCI's February 25th News Release noted (in part):
"The Obama Administration has emphasized reducing fraud, waste, and abuse in Federal entitlements. AdvanceMed is ideally positioned to support the program integrity initiatives of CMS and other Federal Government agencies. . . We are extremely pleased to have AdvanceMed join NCI and believe that this acquisition will provide NCI an outstanding platform to address this rapidly growing market opportunity." (A complete account of NCI's announcement can be found at the above link).
In recent years, AdvanceMed has positioned itself to where it now has multiple contracts with the Federal government. In addition to serving as a Zone Program Integrity Contractor (ZPIC) for Zone 2 and Zone 5, the contractor also serves as Program Safeguard Contractor (PSC) in areas not yet converted to the ZPIC system of contractor review. Additionally, the contractor also serves as a Comprehensive Error Rate Testing (CERT) contractor. On the Medicaid side, AdvanceMed also serves as a Medicaid Integrity Contractor (MIC). While a host of other contractors have been awarded contracts covering other zones and program areas, AdvanceMed’s growth has been undeniably impressive. As NCI announced as part of April 4th "News Release" covering the acquisition:
"AdvanceMed is a premier provider of healthcare program integrity services focused on the detection and prevention of fraud, waste, and abuse in healthcare programs, providing investigative services to the Centers for Medicare and Medicaid Services (CMS). Serving CMS since 1999, AdvanceMed has grown rapidly, demonstrating the value and return on investment of the Federal Government's integrity program activities.
AdvanceMed employs a strong and experienced professional staff, which leverages sophisticated information technology, data mining, and data analytical tools, to provide a full range of investigative services directed to the identification and recovery of inappropriate Medicare and Medicaid funds. AdvanceMed supports healthcare programs in 38 states with a staff of more than 450 professionals, including information specialists, nurses, physicians, statisticians, investigators, and other healthcare professionals.
AdvanceMed has multiple contracts with CMS under the Zone Program Integrity (ZPIC), Program Safeguard (PSC), Comprehensive Error Rate Testing (CERT), and Medicaid Integrity (MIC) programs. All of these programs are executed under cost plus contract vehicles. The largest contracts-ZPIC Zone 5 and ZPIC Zone 2-were awarded in late 2009 and 2010 and have five-year periods of performance.
The acquisition price was $62 million. Included within the price is a recently completed, state-of-the-art data center to support the ZPIC Zone 5 and ZPIC Zone 2 contracts. Additionally, NCI will make a 338(h)(10) election, enabling a tax deduction, which is expected to result in a tax benefit with an estimated net present value of approximately $6 million to $8 million. NCI expects the transaction to be slightly accretive to 2011 earnings.
As of the end of March 2011, AdvanceMed has a revenue backlog of approximately $300 million with approximately $51 million of that amount being currently funded. Revenue for the trailing 12 months ending March 31, 2011, is estimated to be approximately $51 million, all of which was generated from Federal Government contracts, and 99% of the work performed as a prime contractor. NCI's AdvanceMed 2011 revenue, covering the nine-month period of April 2, 2011, to December 31, 2011, is estimated to be in the range of $43 million to $47 million (the equivalent of $57 million to $63 million on a full 12-month basis), with the midpoint reflecting a full-year growth of approximately 16%. . . " (A complete account of NCI's statement can be found at the link indicated above).
II. Overview of the ZPIC Program:
The following comments are intended to provide an overview of the ZPIC program and is not focused on any ZPIC in particular. Under the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MMA), CMS was required to take a number of steps intended to streamline the claims processing and review process:
Using competitive measures, CMS was required to replace the current Medicare Fiscal Intermediaries (Part A) and Carriers (Part B) contractors with Medicare Administrative Contractors (MACs).
After setting up the new MAC regions, CMS created new entities, called Zone Program Integrity Contractors (ZPICs)
These actions were intended to consolidate the existing program integrity efforts. Over the last 2 -- 3 years, ZPICs have been taking over PSC audit and enforcement activities around the country.
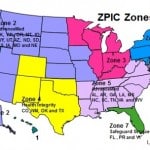
At the time of transition, there were twelve PSCs that had been awarded umbrella contracts by CMS. As these contracts have expired, CMS has transferred the PSCs’ fraud detection and deterrence functions over to ZPICs. Of the seven ZPIC zones established in the MMA, CMS has awarded contracts for a number of the zones. CMS is still working to issue awards for the final ZPIC zones. The seven ZPIC zones include the following states and / or territories:
- Zone 1 – CA, NV, American Samoa, Guam, HI and the Mariana Islands.
- Zone 2 – AdvanceMed: AK, WA, OR, MT, ID, WY, UT, AZ, ND, SD, NE, KS, IA, MO.
- Zone 3 – MN, WI, IL, IN, MI, OH and KY.
- Zone 4 – Health Integrity:CO, NM, OK, TX.
- Zone 5 – AdvanceMed: AL, AR, GA, LA, MS, NC, SC, TN, VA and WV.
- Zone 6 - PA, NY, MD, DC, DE and ME, MA, NJ, CT, RI, NH and VT.
- Zone 7 –SafeGuard Services: FL, PR and VI.
In many instances, these changes have been more of a "name change" rather than a substantive change in the way claims will be audited. ZPIC responsibilities are generally the same as those currently exercised by PSCs. While ZPIC overpayment review duties have not appreciably changed, the number of civil and criminal referrals appear to be increasing. In our opinion, ZPICs clearly view their role differently than that of their PSC predecessors. ZPICs clearly view themselves as an integral part of the law enforcement team, despite the fact that they are for-profit contractors. In consideration of their ability to recommend to CMS that a provider be suspended or have their Medicare number revoked, and / or refer a provider to law enforcement for civil and / or criminal investigation, providers should take these contractors quite seriously.
Both ZPICs and PSCs have traditionally asserted that unlike their RAC counterparts, they are not "bounty hunters." ZPICs are not paid contingency fees like RACs but instead directly by CMS on a contractual basis. Nevertheless, common sense tells us that if ZPICs aren’t successful at identifying alleged overpayments, the chances of a ZPIC’s contract with CMS being renewed are likely diminished. Additionally, experience has shown us that despite the fact that ZPICs are expected to adhere to applicable Medicare coverage guidelines, a ZPIC’s interpretation and application of these coverage requirements may greatly differ from your understanding of the same provisions. In recent years, ZPICs have been aggressively pursuing a wide variety of actions, including but not limited to:
- Prepayment Audit. After conducting a probe audit of a provider’s Medicare claims, the ZPIC may place a provider on "Pre-payment Audit" (also commonly referred to as Prepayment Review). Unlike a postpayment audit, there is no administrative appeals process that may be utilized by a provider for relief. Having said that, there are strategies that may be utilized by a provider which may assist in keeping the time period on prepayment review at a minimum.
- Postpayment Audit. Audits conducted by ZPICs primarily involve Medicare claims that have already been paid by the government. After reviewing these claims, it is not uncommon for a ZPIC to find that the audited provider has been overpaid. Having said that, the ZPICs we have dealt with appear to apply a strict application of the coverage requirements, regardless of whether a provider's deviation from the rules is "de minimus" in nature. In doing so, it is not unusual to find that a provider has failed to fully comply with each and every requirement. Depending on the nature of the initial sample drawn, a ZPIC may extrapolate the damages in a case, significantly increasing the alleged overpayment. In doing so, the ZPIC is effectively claiming that the "sample" of claims audited are representative of the universe of claims at issue in an audit.
- Suspension. While the number of suspension actions taken by ZPICs has steadily increased in recent years, Medicare providers should expect to see this number continue to grow. Under the Affordable Care Act (often informally referred to as the "Health Care Reform" Act), CMS’ suspension authority has greatly expanded.
- Revocation. As with suspensions, we have seen a sharp increase in the number of Medicare revocation actions taken over the last year. The reasons for revocation have varied but have typically been associated with alleged violations of their participation agreement. In some cases, the ZPIC contractors found that the provider has moved addresses and did not properly notified Medicare. In other cases, a provider was alleged to have been uncooperative during a site visit. Finally, there were a number of instances where the provider allegedly did not meet the "core" requirements necessary for their facility to remain certified.
- Referrals for Civil and Criminal Enforcement. ZPICs are actively referring providers to the OIG (which can in turn refer the case to the U.S. Department of Justice for possible civil and / or criminal enforcement) when a case appears to entail more that a mere overpayment. However, just because a referral is made doesn’t mean that it will prosecuted. In many instances, OIG (and / or DOJ) will decline to open a case due to a variety of reasons, such as lack of evidence, insufficient damages, etc.).
III. Steps Providers Can Take Now, Before They are Subjected to a ZPIC Audit:
In responding to a ZPIC audit, it is important to remember that although they may not technically be "bounty hunters," it is arguably to their benefit to find that an overpayment has occurred. These overpayments are often based on overlapping "technical" (such as an incorrect place of service code) and "substantive" (such as lack of medical necessity) reasons for denial. In recent years, the level of expertise exercised by ZPICs is often quite high -- noting multiple reasons for denial and concern.
Unfortunately, the reality is that most (if not all) Medicare providers will find themselves the subject of a ZPIC, CERT, RAC or other type of claims audit at some point in the future. In our opinion, the single most effective step you can take to prepare for a contractor audit is to ensure that your organization has implemented and is adhering to an effective Compliance Plan. A comprehensive assessment of an organization's coding and billing practices is one element of an effective plan. Several general points to consider also include:
Keep in mind your experiences with PSCs and other contractors. The lessons you have learned responding to PSC, CERT and RAC audits can be invaluable when appealing ZPIC overpayments. As you will recall, the appeals rules to be followed are virtually the same.
Monitor OIG’s Work Plan. While often cryptic, it can be invaluable in identifying areas of government concern. Are any of the services or procedures your organization currently provides a focus of HHS-OIG’s audit or investigative?
Keep an eye on RAC activities. Review the service-specific findings set out in annual RAC reports. Review targeted areas carefully to ascertain whether claims meet Medicare’s coding and medical necessity policies.
You never realize how bad your documentation is until your facility is audited. While many providers start out "over-documenting" services (to the extent that there is such a thing), a provider’s documentation practices often become more relaxed as time goes on – especially when the provider has not been audited for an extended period of time. In such situations, both physicians and their staff may fail to fully document the services provided. Moreover, the care taken to ensure that all supporting documentation has been properly secured may have also lapsed over the years.
Review your documentation. Imagine you are an outside third-party reviewer. Can an outsider fully appreciate the patient’s clinical status and the medical necessity of treatment? Are the notes legible and written is a clear fashion? Compare your E/M services to the 1995 or 1997 Evaluation and Management (E/M) Guidelines – have you fully and completely documented the services you provided? If dealing with skilled services, have you fully listed and discussed both the need for skilled services and the specific skilled services provided?
IV. Closing Thoughts on NCI-Owned AdvanceMed:
Imagine a ZPIC hands you a claims analysis rife with alleged errors, an indecipherable list of statistical formulas, and an extrapolated recovery demand that will cripple your practice or clinic. What steps should you take to analyze their work? Based on our experience, providers can and should carefully assess the contractor’s actions, particularly the use of formulas and application of the RAT-STATS program when selecting a statistical sample and extrapolating the alleged damages based on the sample. To be clear, not all statistical extrapolations will be flawed. Depending on the steps taken by the ZPIC's statistician, to the Over the years, we have challenged the extrapolation of damages conducted by Medicare contractors around the country, including tens of thousands of claims. Regardless of whether you are a Skilled Nursing Facility providing skilled nursing and skilled therapy services, an M.D. or D.O. providing E/M services, a Home Health company or a Durable Medical Equipment (DME) company, it is imperative that you work with experienced legal counsel and statistical experts to analyze the actions take by a ZPIC.

Liles Parker attorneys and staff have extensive experience representing a wide range of Medicare providers in audits by ZPICs and other CMS program integrity contractors. Should you have questions regarding an inquiry from a ZPIC or RAC that you have received, please feel free to give us a call for a complimentary consultation. We can be reached at: 1 (800) 475-1906.
