
(March 16, 2016): Last week, the Centers for Medicare & Medicaid Services (CMS) released a new dataset which provides detailed information on services provided by skilled nursing facilities (SNFs) to Medicare beneficiaries. This data set is known as the “Skilled Nursing Facility Utilization and Payment Public Use File” (SNF PUF), as is part of CMS’s Medicare Provider Utilization and Payment Data sets. Notably, this newly-released data includes information on 15,055 SNFs. During the period at issue (2013), these 10,005 SNFs billing the Medicare program for more than 2.5 million stays, and received almost $27 billion in Medicare reimbursement. As the SNF PUF data reflects, payments for ultra high therapy billing claims were the largest made to SNFs by Medicare during this period. As CMS has announced, these therapy billing practices will be carefully scrutinized by Medicare contractors. The purpose of this article is to discuss the nature of the audits that Texas SNFs should expect in the near future.
I. What Constitutes “Ultra High Therapy Billing”?
SNFs are reimbursed under the Medicare program under a prospective payment system. Under this type of payment system, SNFs classify each Medicare beneficiary into one a specific Resource Utilization Group (RUG), based on the patient’s individual care and resource needs. Each RUG is reimbursed by Medicare at a different per diem rate. While only a portion of the RUG codes are used to categorize Medicare SNF patients who need therapy, the remaining RUG codes are used to categorize Medicare SNF patients who require little or no therapy. As you would expect, Medicare’s reimbursement rates for RUGs which require therapy are generally higher than those for non-therapy RUGs.
Within the RUG therapy categories, Medicare SNF patients who require higher levels of therapy receive the most reimbursement. SNFs categorize Medicare beneficiaries needing therapy into different levels, based (mostly) on the number of therapy minutes needed and administered. Medicare SNF patients who receive the highest number of minutes of therapy likely qualify for placement in an ultra high therapy RUG.
II. Background of SNF Ultra High Therapy Billing Concerns:
At the outset, it is important to keep in mind that the government has long expressed concern over the billing of ultra-high therapy services. In December 2010, the Department of Health and Human Services, Office of Inspector General (HHS-OIG), issued its report entitled “Questionable Billing by Skilled Nursing Facilities,” (OEI-02-09-00202). As HHS-OIG detailed in its report:
- From 2006 to 2008, SNFs increasingly billed for higher paying RUGs, even though beneficiary characteristics remained largely unchanged. While the ages and diagnoses of Medicare SNF patients remained constant from 2006 to 2008, the percentage of RUGs for ultra high therapy increased from 17 to 28 percent.
- For-profit SNFs were far more likely than nonprofit or government SNFs to bill the Medicare program for higher paying RUGs. During the period under review, 32% of the RUG claims submitted to Medicare from for-profit SNFs were for ultra high therapy. In contrast, during this same period, only 18% of the RUG claims from non-profit SNFs and 13% of the RUG claims from government-run SNFs were for ultra high therapy.
In November 2012, HHS-OIG issued its report entitled “Inappropriate Payments to Skilled Nursing Facilities Cost Medicare More than a Billion Dollars in 2009,” (OEI-02-09-00200). This report was based on a medical record review conducted by HHS-OIG of a stratified random sample of SNF claims from 2009. The purpose of the medical record review was to assess whether the information reported by the SNFs on the Minimum Data Set (MDS) was supported by and consistent with each patient’s medical record. The MDS is a standardized tool that SNFs use to assess the care and resource needs of each Medicare patient. SNFs use the MDS data to categorize each patient into the proper RUG level. As HHS-OIG reported:
“SNFs billed one-quarter of all claims in error in 2009, resulting in $1.5 billion in inappropriate Medicare payments. The majority of the claims in error were upcoded; many of these claims were for ultra high therapy. The remaining claims in error were downcoded or did not meet Medicare coverage requirements. In addition, SNFs misreported information on the MDS for percent of claims. SNFs commonly misreported therapy, which largely determines the RUG and the amount that Medicare pays the SNF.” (Emphasis Added).
Late last year, HHS-OIG followed-up these earlier reports and issued the results of its latest review of SNF Medicare claims. In its September 2015 report entitled, “The Medicare Payment System for Skilled Nursing Facilities Needs to be Reevaluated,” (OEI-02-13-00610), HHS-OIG reached several conclusions:
- Medicare payments for therapy greatly exceeded SNFs’ costs for therapy.
- Under the current payment system, SNFs increasingly billed for the highest level of therapy even though key beneficiary characteristics remained largely the same.
- Increases in SNF billing—particularly for the highest level of therapy—resulted in $1.1 billion in Medicare payments in FYs 2012 and 2013.
III. Current Concerns with SNF Ultra High Therapy Billing Practices:
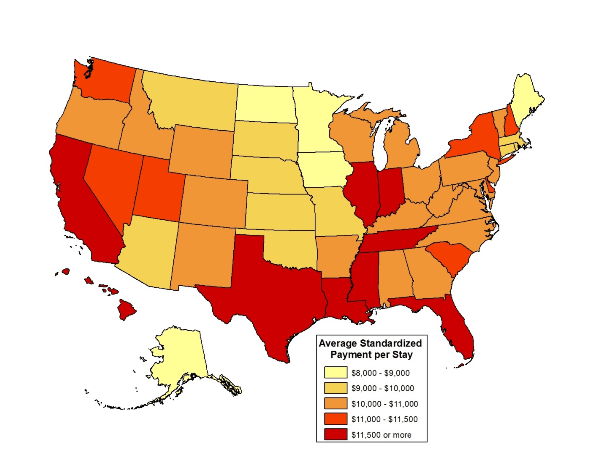
Most recently, in the SNF PUF report issued by CMS last week, the agency confirmed that SNF ultra high therapy billing practices remains a significant problem. The SNF PUF report was culled from Medicare claims data from 15,055 SNFs and more than 2.5 million stays, also compared SNF costs and utilizations by geographic area. As CMS further found, on a national basis, the average standardized payment amount per stay for all SNFs was $10,919, with an average length of stay of 28 days. Notably, Texas was one of the states with the highest average standardized payment amounts per stay -- $12,064.
IV. What Should SNFs Expect in the Future?
As outlined in a Press Release issued by CMS on March 9, 2016, the agency intends to “step-up” its audit efforts of ultra high SNF therapy claims. According to the release:
“CMS strives to ensure that patient need, rather than payment system incentives, are driving the provision of therapy services,” says Dr. Shantanu Agrawal, Deputy Administrator for Program Integrity and Director of the Center for Program Integrity. “These concerns have prompted us to refer this issue to the Recovery Auditor Contractors (RAC) for further investigation, and our hope is that data transparency will facilitate real changes.” (Emphasis Added).
Importantly, there is no requirement that CMS make a specific referral to Zone Program Integrity Contractors (ZPICs) in order for them to initiate additional audits and investigations into the billing and utilization practices of SNF ultra high therapy claims. In recent years, we have seen a number of SNF ZPIC audits, many of which ultimately alleged that the provider had improperly billed for ultra therapy claims. SNF providers should expect for the number of ZPIC audits focused on ultra high Medicare claims to increase over the next year. Coupled with the anticipated increase in RAC audits of these claims, SNF provider therapy claims will likely be under considerable scrutiny for the immediate and near future.
V. Conclusion:
What steps can your SNF take to minimize potential overpayment liability? As a first step, we recommend that you determine how your SNF’s payment and utilization rate compare with those of its peer institutions and / or other SNFs in your state? CMS has broken down the SNF PUF into five tables. These tables include: (1) aggregated information by provider, (2) aggregated information by provider and RUG, (3) aggregated information by RUG, (4) aggregated information by RUG and state, and (5) aggregated information on therapy minutes by provider. This information can be invaluable in helping you determine whether the RUG claims you are billing are consistent with what would normally be expected or whether your billing practices would likely be viewed as an outlier. While these numbers are helpful, at the end of the day an audit is going to focus on whether the therapy services were medically necessary, meet applicable documentation requirements and ultimately qualify for coverage and payment. Our attorneys have extensive experience analyzing SNF therapy claims and can assist you in conducting a preemptive review of your practices.

