
(January 26, 2018): From Churches to Congress, sexual harassment and assault charges have plagued many of the institutions that our society holds dear. As revelations of sexual misconduct continue to surface, we continue to learn of the many abuses of those in powerful positions; those whom we once revered. The rise of the #MeToo Movement ("Movement") in late 2017 has brought about a national conversation over sexual assault and harassment. Women and men from all industries have been revealing tragic stories of sexual assault and harassment. Not surprisingly, healthcare practices and organizations haven’t been immune to this societal crisis. In fact, it now appears that sexual assault and harassment may be far more prevalent in medicine than has been previously acknowledged. Recent studies have exposed that sexual misconduct by physicians is not only more common than previously thought, but also poorly disciplined when acknowledged.
In this article, we have collected data on disciplinary actions for sexual misconduct by physicians in Texas throughout 2017.[1] This article breaks down the 2017 disciplinary actions into (1) the different forms of sexual misconduct cited, (2) the physician specialties involved, (3) the time frame of the disciplinary actions, and (4) the severity of the disciplinary action taken by the Texas Medical Board (“Board”) against the subject physician. Prior to examining the data, let’s delve into the #MeToo Movement and the prevalence and discipline of sexual misconduct in medicine.
I. What is the #MeToo Movement?
The #MeToo Movement as we know it today emerged out of the revelations last October of sexual abuse by powerful men in the Hollywood and entertainment industry.[2] Since the first allegations surfaced, more and more powerful people, particularly men, have been exposed and alleged to have committed various types of sexual assault, harassment or other improper conduct. To many, the sheer volume of sexual misconduct allegations exposed has come as a great shock. The #MeToo Movement has showed us that perpetrators of sexual misconduct can be practically anyone. Celebrities, athletes, government officials, and otherwise seemingly ordinary individuals have all been named as wrongdoers. To the extent that there is one, the silver lining of the #MeToo Movement is that it has empowered women to stand up for their rights and it has initiated a national self-evaluation on what is (and isn’t) appropriate interpersonal conduct between adults in the workplace. Ultimately, we will all benefit from this conversation.
II. An Overview of the Problem
At present, 1 in 5 women in the United States will be raped in their lifetime and nearly 1 in 2 women in the United States will be victims of sexual misconduct other than rape.[3] In accordance with the later statistic, 13% of women in the United States will be sexually coerced, 27.2% will be sexually assaulted, and 33.7% will be sexually harassed.[4] Despite the alarming prevalence, rape and sexual assault is the lowest reported crime, with an estimated 67% of victims not reporting their crime to the police.[5] In the workplace, the Equal Employment Opportunity Commission (EEOC) estimates that 75% of sexual harassment goes unreported. [6] This is often attributed to the stigma and lack of support that victims face in society. However, through raising awareness of the prevalence of this issue, the #MeToo Movement is expected to ignite social progress towards supporting victims and taking action against perpetrators. It is reasonably expected that this Movement will continue to empower many more victims to report to various authorities, whom will be expected to take further action to prevent and stop sexual misconduct.
III. What Constitutes Sexual Harassment / Sexual Misconduct?
As you can imagine, there is no single definition of the terms “sexual harassment” or “sexual misconduct.” Moreover, there isn’t even agreement on when one of these specific terms should apply. Rather than get bogged down in semantics or spend all day comparing and contrasting how different courts have defined these terms, for the purposes of this article, we intend to utilize the terms interchangeably.
The term, “sexual harassment.” is defined at by the EEOC as the harassment of:
“[A] person… because of that person’s sex. Harassment can include “sexual harassment” or unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment of a sexual nature… Both victim and the harasser can be either a woman or a man, and the victim and harasser can be the same sex”. [7] (emphasis added).
In contrast, the Federation of State Medical Boards has adopted a more specific definition of the term that is focused on the physician-patient relationship. The Federation of State Medical Boards defines physician sexual misconduct as:
“[B]ehavior that exploits the physician-patient relationship in a sexual way. Sexual behavior between a physician and a patient is never diagnostic or therapeutic. This behavior may be verbal or physical, and may include expressions of thoughts and feelings or gestures that are sexual or that reasonably may be construed by a patient or patient’s surrogate as sexual”. [8] (emphasis added).
According to sections 22.011 and 22.021 of Chapter 22 of the Texas Penal Code, sexual assault includes all physical contact of a sexual nature in which consent was not or could not be given. Sexual misconduct is most often predicated on a power dynamic between the perpetrator and the victim.[9] In medicine, the physician holds power over their patients and subordinates. Thus, this power dynamic between perpetrator and victim makes it such that consent is not a defense for physicians.[10] The Texas Penal Code specifically addresses this dynamic in Chapter 22, Section 22.011 (b)(9), which states that the act is not consensual if:
“[T]he actor is a mental health services provider or a health care services provider who causes the other person, who is a patient or former patient of the actor, to submit or participate by exploiting the other person’s emotional dependency on the actor;” (emphasis added).
How does your health care practice or organization define sexual harassment or sexual misconduct? Regardless of the definition ultimately adopted, there are a number of examples of conduct that are generally recognized as problematic. These include, but are limited to:
- Sexual jokes, pranks or teasing. This conduct can expressly allude to sexual matter or can refer to sex by innuendo. It can be made in person, over the phone by e-mail, or by some other method of communication.
- Touching, grabbing or making pretend motions or gestures of a sexual nature.
- Verbally engaging in sexually discussions or making sexually charged comments at the workplace.
- Repeatedly standing too close to a person, brushing up against them or otherwise getting in their personal space and making them uncomfortable.
- Showing or otherwise posting sexually demeaning or offensive pictures, cartoons, comments or other materials in the workplace.
- Repeatedly asking someone to socialize during off-duty hours when he or she has already that he / she is not interested in engaging in social activities.
- Giving gifts or leaving objects that are unwanted, regardless of whether they are sexually suggestive.
- Asking about someone’s sexual experiences or preferences and / or discussing your own sexual experiences, activities and / or preferences.
IV. Generally Speaking, how Common is Sexual Misconduct in Medicine?
As an elite profession, physicians are revered and given an elevated status. As far back as Ancient Greece, physicians have sworn oaths that forbade engaging in any form of sexual misconduct.[11] Despite moral and ethical oaths, this “elite” status is easily manipulated by perpetrators, especially against patients. In a 2016 report, the Atlanta Journal-Constitution uncovered that hidden and pervasive nature of sexual misconduct in medicine. Since 1999, more than 3,100 physicians have been formally accused of sexual misconduct, with at least 2,400 of those physicians engaging in sexual misconduct with patients. It is important to note that this makes up an extreme minority within the over 950,000 physicians practicing in the United States. However, akin to prior sexual misconduct scandals, one perpetrator is capable of routinely victimizing patients. In one particular case, a pediatrician sexually assaulted at least 1,200 children over 15 years. [12] However, most of the 3,100 perpetrators did not target children, but rather young women.
In all, the actual details on the prevalence of sexual misconduct are difficult to accurately unearth for a multitude of reasons. Doctors are viewed as educated and credible, giving way to a predisposition by authorities to believe the word of the physician over an alleged victim. Additionally, most states do not post rather detailed public records related to sexual misconduct. [13] The details of allegations are often left out or obscured, leaving the public with little knowledge of what any given physician may have done. Some state medical boards choose not to publicly release information about a first-time offense. Additionally, when the evidence is discovered through a peer-review at the medical institution, state laws often prohibit that information from being shared. To make matters worse, inadequate screening procedures prevent some state medical boards from discovering prior allegations made against physicians, allowing some perpetrators to move to a new location and continue to victimize patients and coworkers.
V. How is Sexual Harassment and Misconduct Disciplined in Medicine?
While state medical boards claim to take sexual misconduct seriously, the Atlanta Journal-Constitution seems to tell another tale. Of the 3,100 physicians disciplined for sexual misconduct since 1999, 2/3 were permitted to continue practicing.[14] In the case of some serial predators, this meant they could continue to victimize their patients and coworkers with no serious repercussions. The report found that cases were obscured as were disciplines. Not all cases of sexual assault and harassment were labeled as such, many were marked in general terms such as crossing “boundaries” or having a “sexual relationship” with a patient. In most states, state medical boards and healthcare institutions choose to make compromises with the physician in order to avoid protracted legal battles. This is because state medical boards can only operate within the statutory authority given by that state’s legislature. Thus, patient protection may be a priority for state medical boards, but they can only work within the framework provided to them. In addition, some state medical boards view the physicians as a scarce public health resource. In some rural areas, state medical boards have weighed the implications of removing a physician’s license on the ability of the populace to seek out a physician.
The actual disciplinary actions taken seem to echo past sexual misconduct scandals. Disciplinary actions are overwhelmingly aimed at rehabilitation rather than punishment. Physicians are frequently seen not as criminals, but rather as individuals suffering from mental illness. These disciplinary actions aimed at educating physicians on sexual misconduct, legal repercussions, and their “boundaries” with patients and coworkers. Many have been sent to “treatment,” as state medical boards seek to salvage the value they see in physicians. Many are even given the restriction of a required chaperone while they are seeing patients of the opposite sex. Not all disciplinary actions are as bleak for patient protection. Many of these perpetrators have been fined, publicly reprimanded, had their license suspended or restricted, or lost their license all together. Voluntary surrender does unfortunately offer perpetrators the ability to avoid further investigation. However, some state medical boards have also adopted the policy of revoking a medical license if that individual surrenders their license in another state in lieu of sexual misconduct allegations.
VI. How Well Does Texas Protect its Patients?
In conjunction with their damning report, the Atlanta Journal-Constitution also created a “report card” for how well each state protects its patient from sexual misconduct by physicians. Each state received a numerical score from 0-100, averaged from a similar scale judging the state’s transparency, duty-to-report laws, board composition, criminal acts, and discipline laws. The best state was Delaware, while the worst state was Mississippi. Since our research focused on the Texas Medical Board, we will examine the Texas State Report Card.
The good news is that Texas ranked second, with an overall rating of 80. Texas ranked as the most transparent state, with a score of 90. Though hospital sanctions are not listed, the Texas Medical Board maintains an accessible public record for all Board orders that provides details as to why Board orders were taken.
Unfortunately, the “duty-to-report” laws in Texas were not adjudged by Atlanta Journal-Constitution to be quite as superb. Texas was given a score of only 52 due to insufficient reporting laws. Hospitals are required to report the details of a peer review that results in a more than 30-day suspension, or when a physician surrenders their clinical privileges in exchange for not conducting an investigation. However, if a physician is disciplined for 30 or fewer days, the details are not required to be released. Additionally, there is no deadline for how long a hospital can wait to report, nor are there legally established repercussions for a failure to do so. Courts are not required to notify the Board of criminal convictions. Fellow physicians, however, are required by law to report any behavior by peers that may pose a threat to the public welfare.
The Board composition score was slightly better, at 70. It is comprised of 19 total individuals including 7 consumers with no immediate or marital relation to medicine and 12 physicians. Only 3 of the 19 board members are female.
The criminal acts score for Texas is remarkably high, at 96. This is primarily because the Texas Medical Board requires a thorough background check for applicants, then continues to periodically monitor criminal records of licensed physicians. Additionally, state law requires that the board report criminal conduct to police. As mentioned earlier, Texas has also criminalized sexual misconduct by physicians by removing consent as a legal defense.
Lastly, Texas tied Delaware and Alaska for the highest score for discipline laws with a score of 90. As per state law, the Board must revoke any license for a felony conviction or a deferred adjudication involving sexual abuse of a child. However, this revocation is not permanent unless the physician agrees to that stipulation or permanently surrenders their license in lieu of further investigation. State law also requires that an applicant cannot be licensed if their license elsewhere is currently restricted, cancelled, suspended, or revoked. State law also prohibits licensing any applicant that is being prosecuted for a crime that, if prosecuted in Texas, would be felony or misdemeanor involving moral turpitude. In addition, the board may subpoena hospitals for peer review records and the standard of proof for board action is only a preponderance of evidence.
Overall, the Texas Medical Board is amongst the best in the nation at handling formally submitted complaints of sexual misconduct by physicians. However, that bar is still too low. Finding records of allegations remains difficult in Texas. Additionally, anonymous reporting is not permitted, likely contributing to some victims deciding not to report.
VII. Texas Medical Board Disciplinary Actions for Sexual Conduct in 2017:
In 2017, the Texas Medical Board took 18 total disciplinary actions against 17 physicians for sexual misconduct. Six physicians were disciplined for sexual assault, with 2 of the 6 also being disciplined for sexual harassment. The disciplinary action imposed by the Board in each of these actions except for one, was a suspension of the physician’s medical license. The one outlier was a physician who voluntarily surrendered his license in lieu of investigation; this physician’s license had previously been suspended earlier in 2017 for sexual assault. Only one physician was disciplined for sexual harassment alone, which resulted in sanctions which including taking a medical jurisprudence exam and multiple educational courses. Two physicians were disciplined for sexual misconduct, though both actions were a result of actions by other institutions. In the first case, the Board found that one physician failed to report disciplinary action by his alma mater for sexual misconduct. This resulted in a fine and mandatory educational courses. The second case involved a physician licensed in Texas but practicing in Oklahoma. This individual’s license was revoked in Texas following the voluntary surrender of his license in Oklahoma due to pending sexual assault charges. The remaining sexual misconduct-related disciplinary actions were referred to as having a “sexual relationship with a patient.” All but one of these cases resulted in a punishment that included mandatory continuing education. Five of these disciplinary actions resulted in public reprimands. Other forms of disciplinary action taken in these cases included fines, chaperones while with female patients, a medical jurisprudence exam, psychiatric treatment, and a temporary license restriction.[15]
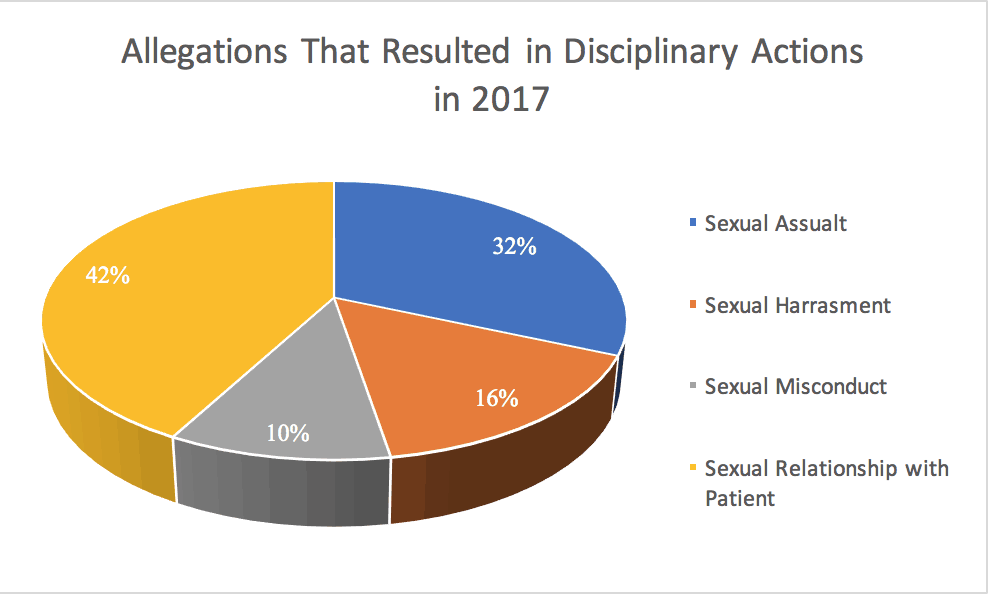
Figure 1: Allegations that resulted in disciplinary actions taken by the Texas Medical Board in 2017.[16]
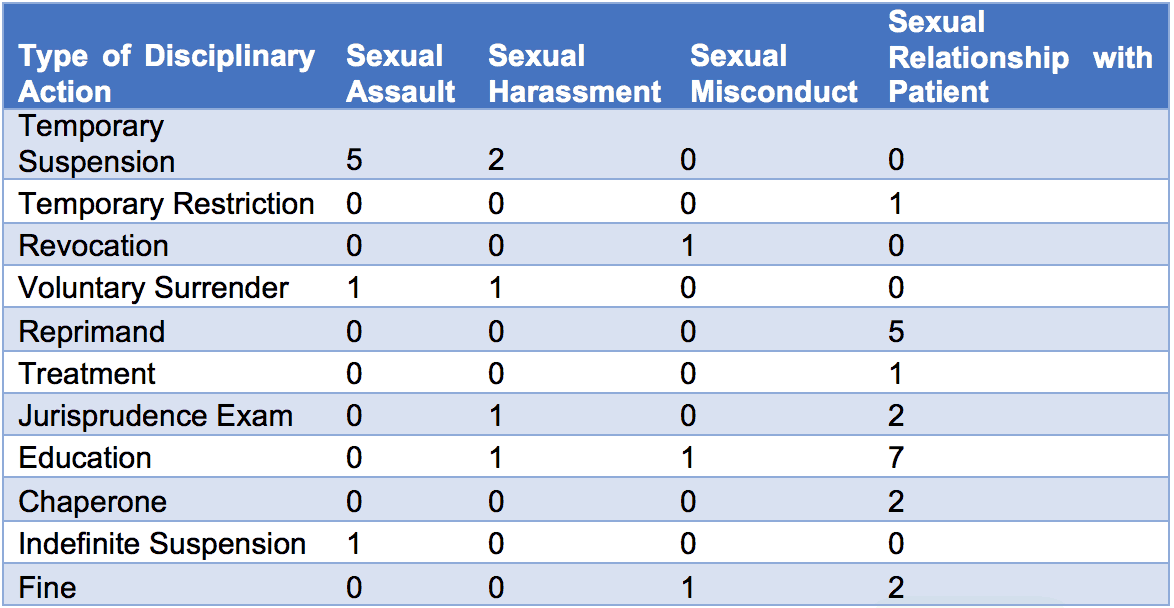
Table 1: Types of disciplinary actions taken by the Texas Medical Board in 2017 for each type of allegation.[17]
There did not appear to be any large trends within the type of physician specialty. The most common specialty was internal medicine, with a total of 5 internists out of 17 total disciplined physicians. No significant geographical trend was observed, with the cases largely spread out amongst relatively populated areas of Texas. Over 50% of the disciplinary actions occurred in the first half of the year. Surprisingly, there was no particular increase in disciplinary actions following the rise of the #MeToo Movement in October 2017.
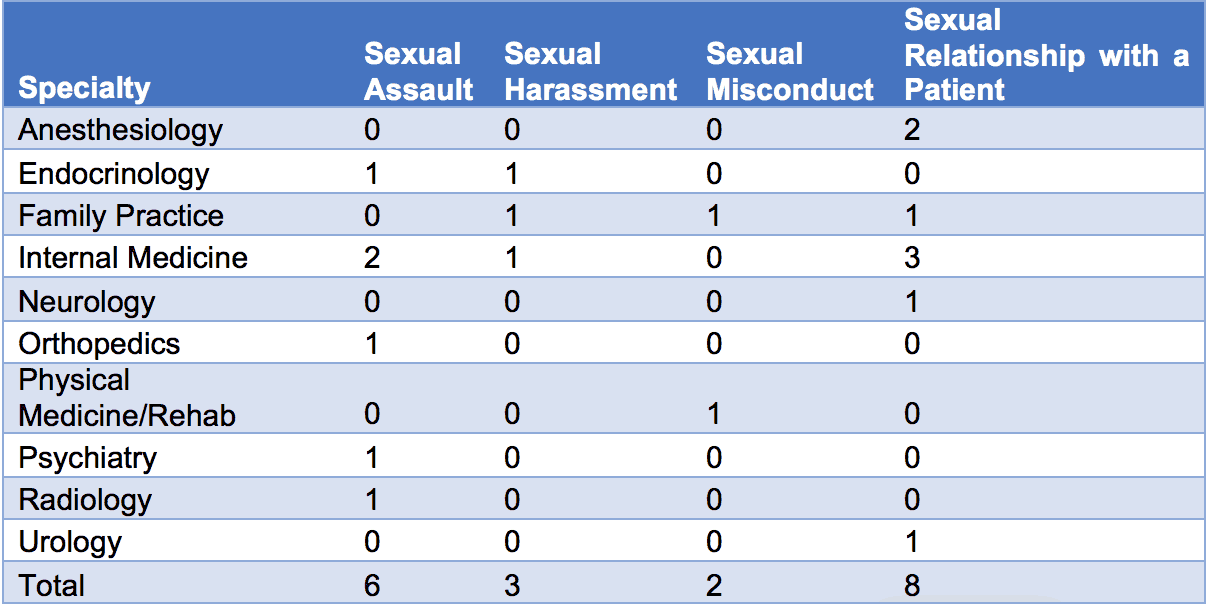
Table 2: Allegations that resulted in disciplinary action by physician specialty.[18]
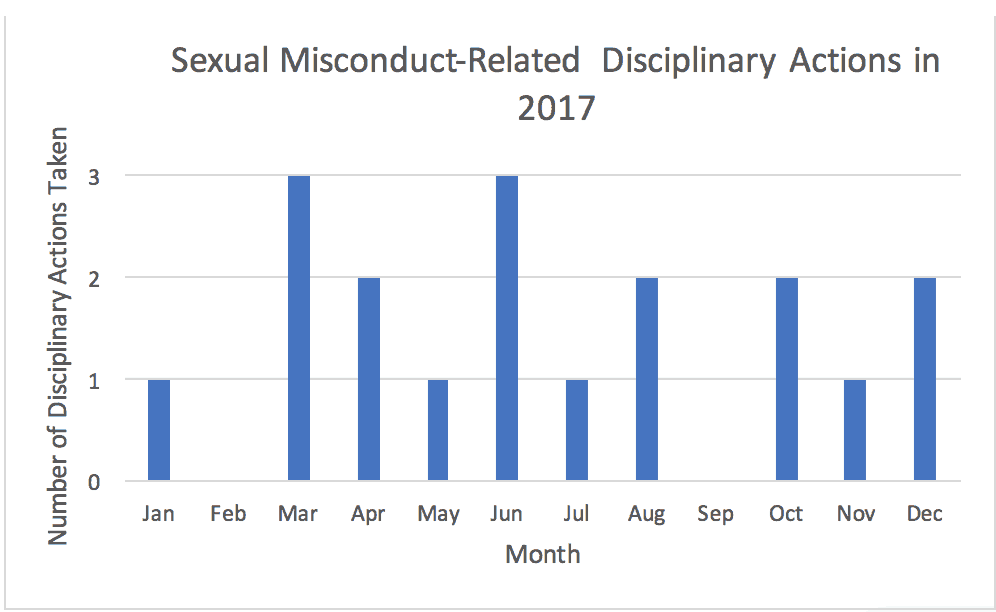
Figure 2: Sexual misconduct-related disciplinary actions taken each month by the Texas Medical Board in 2017.[19]
VIII. The Texas Medical Board Weighs In on Sexual Harassment Complaints:
In the January 2018 Texas Medical Board Bulletin, two interesting topics appear on Page 3 and 4: the use of chaperones and duty to report impairment. Each bulletin published offers news and reminders relevant to hot topics. Most bulletins in the last 5 years have covered topics related to prescription drugs, but none of those bulletins have covered either of these topics. It is worth noting that this is the first bulletin to be published since the #MeToo campaign began.
The first of the seemingly relevant topics is the use of chaperones. This section seeks to remind physicians that there are many ways to ""make patients feel comfortable during their visit;" highlighting the use of a chaperone as one particularly ethical method of doing so, in addition to providing gowns and using drapes. The second seemingly relevant topic was the duty to report impairment. As addressed earlier in this article, state medical boards frequently view perpetrators of sexual misconduct as mentally ill rather than criminals. This section of the January 2018 bulletin seems to echo that narrative, reminding physicians that they may report themselves and fellow physicians that pose a continuing threat to the public welfare. Additionally, it highlights that in certain circumstances, civil liability may be lifted from the reporting party.
While this was not a direct response to the #MeToo Movement, it does appear relevant, and perhaps anticipatory. This bulletin appears to remind physicians that patient comfort and safety is an ethical priority in medicine. Impairment does not automatically indicate sexual misconduct, though sexual misconduct has certainly been attributed to impairment by the board in the past.[20] Through this bulletin, it is plausible to say that the Board may be anticipating, and perhaps encouraging, more reports of sexual misconduct by physicians in the near future.
The #MeToo Movement seems to have struck a chord with the American public. It seems that society may finally begin to address the pervasive nature of sexual misconduct. All of this comes as we learn of tragic stories of abuses and cover ups. Like many other industries, medicine appears to have a dark past of turning a blind eye to physicians who abused patients and coworkers. While the number of physicians engaging in sexual misconduct may be far and few between, their actions have harmed, at the least, thousands of patients and coworkers. As the #MeToo Movement carries into 2018, perhaps we will learn more about the true scale of sexual misconduct in medicine as more victims come forward.
While no state medical board appears to be perfect at addressing sexual misconduct, the Texas Medical Board is currently one of the best. Their 2017 data shows that sexual misconduct appears to be rare amongst physicians in Texas, at least on the surface. Considering how Board investigations into these matters can take months, it is plausible that the 2017 does not reflect the societal shifts in reporting since the beginning of the #MeToo Movement. The Movement may have effectively changed the national environment that felt hostile to most victims. Some have likened its energy of the #MeToo Movement to that of the civil rights movement, hoping that the social media campaign will result in coordinated efforts to achieve legal and cultural reform.[21] With more victims feeling supported, it is almost certainly expected that reports of sexual misconduct will rise across.
If the Movement does translate to more reports of sexual misconduct generally, it is plausible that a better portrait of sexual misconduct in medicine may emerge. Thus, we will conduct this same assessment of the Texas Medical Board’s disciplinary actions against sexual misconduct at the conclusion of 2018. It is likely that more physicians are guilty of sexual misconduct than the Board is aware of or has taken action against. In comparing the 2018 and 2017 results, we will be able to determine how the #MeToo campaign has impacted medicine. We can expect to see more disciplinary action by the Board in 2018. The causes of the disciplinary actions may become less vague and the punishments more severe. For the time being, this is only speculation. Only time will tell how the #MeToo Movement will impact sexual misconduct in medicine.
IX. Healthcare Organizations Need to Conduct a Top-Down Review of Their Policies and Procedures:
Even as state medical boards enact stronger policies against sexual misconduct, it is important to note that the organizations and individuals who failed to adequately prevent, stop, or report sexual misconduct by a physician have been held liable, and will likely continue to be held liable into the future. In the case of the pediatrician who sexually assaulted hundreds of children, the hospital he sometimes worked for, a medical society, and doctors that referred patients to this physician were sued, which was resolved through a final settlement of $122 million for the defendant’s former patients.[22] Therefore, it is important for any organization hoping to avoid liability to create detailed policies and procedures on sexual harassment and sexual misconduct. In doing so, health care organizations should ensure that they are preemptively educating both patients and employees on what constitutes sexual harassment and sexual misconduct and what the ramifications are not only for perpetrators, but also bystanders who do not report. Health care organizations should require reporting such that allegations are not covered up nor overlooked. A low-cost, comprehensive, anonymous reporting system such as that provided by ComplianceHotline.com can provide your practice or other health care organization with a full range of reporting options that can be made available to patients and employees alike if they are concerned about sexual harassment or misconduct.[23] Moreover, this anonymous hotline tracks the recommended steps recommended by HHS-OIG in its recent guidance, “Measuring Compliance Program Effectiveness: A Resource Guide.” The bottom line is straightforward -- encouraging the early reporting of sexual misconduct can significantly reduce your health care entity’s level of regulatory risk and improve the quality of work life for your staff.
Unfortunately, drafting the proper Policies and Procedures to be used in your health care organization can be tricky. You need to take both federal and state requirements into account. Please feel free to contact us for assistance with both the policies and with staff training on these important issues.

- [1] Specifically, we reviewed Texas Medical Board Bulletins posted in April 2017, September 2017, and April 2017.
- [2] https://www.theguardian.com/world/2017/oct/20/women-worldwide-use-hashtag-metoo-against-sexual-harassment
- [3] https://www.nsvrc.org/sites/default/files/nsvrc_one_pager_0.pdf
- [4] https://www.cdc.gov/ViolencePrevention/pdf/NISVS_Report2010-a.pdf
- [5] https://www.bjs.gov/content/pub/pdf/rsarp00.pdf
- [6] http://www.chicagotribune.com/business/ct-biz-metoo-sexual-harassment-future-20171214-story.html
- [7] https://www.eeoc.gov/laws/types/sexual_harassment.cfm
- [8] https://www.fsmb.org/Media/Default/PDF/FSMB/Advocacy/GRPOL_Sexual%20Boundaries.pdf
- [9] https://www.psychologytoday.com/blog/close-encounters/201712/when-do-men-power-engage-in-sexual-harassment
- [10] http://doctors.ajc.com/doctors_sex_abuse/
- [11] http://www.pbs.org/wgbh/nova/body/hippocratic-oath-today.html
- [12] http://doctors.ajc.com/why_abusive_doctors_not_caught/?ecmp=doctorssexabuse_microsite_stories
- [13] http://doctors.ajc.com/states_discipline_sex_abuse/
- [14] http://doctors.ajc.com/doctors_sex_abuse/?ecmp=doctorssexabuse_microsite_nav
- [15]
http://www.tmb.state.tx.us/dl/A1BB2B98-02FD-3A3C-9022-D99248F0EEBF;
http://www.tmb.state.tx.us/dl/B35F98D0-7F66-6F8B-8D5D-6A1520FF9C3F;
http://www.tmb.state.tx.us/dl/209310BC-7307-EF80-6049-3FDC28CF182D - [16] Id.
- [17] Id.
- [18] Id.
- [19] Id.
- [20] https://www.documentcloud.org/documents/2940026-combined-164-pdf.html
- [21] http://www.cnn.com/2017/10/30/health/metoo-legacy/index.html
- [22] https://www.usatoday.com/story/news/nation/2013/11/25/delaware-child-abuse-case-settlement/3720309/
- [23] Paul Weidenfeld and Robert W. Liles established www.compliancehotline.com to provide health care providers and suppliers with a comprehensive anonymous complaint reporting system that could be incorporated into their overall Compliance Program.
