
(June 15, 2023): The Department of Health and Human Services (HHS) is enormous, employing more than 80,000 individuals[1] who work in a dozen operating divisions and an even greater number of independent offices that report directly to the Office of the Secretary.[2] One of these independent offices is the HHS Departmental Appeals Board (DAB or Board). The DAB has been designed to provide an impartial, independent review of disputed agency decisions under a wide variety of statutory and regulatory provisions.[3] This article examines the DAB in more detail, focusing on the Board’s appellate role when adjudicating exclusion, provider enrollment actions and HIPAA administrative simplification violations.
I. History of the Departmental Appeals Board:
While in its earlier incarnation as the Department of Health, Education and Welfare (HEW), the Secretary, HEW first established an entity known as the Departmental Grants Appeals Board in 1973.[4] At that time, HEW was the first Federal grantor agency to create a structured process for resolving administrative disputes. In 1980, HEW was renamed the Department of Health and Human Services (HHS). The Departmental Grants Appeals Board was subsequently renamed the Departmental Appeals Board and its limited jurisdiction over grant programs was greatly expanded to include a wide variety of HHS related programs. For example:
- 1988: The Secretary, HHS, delegated to the Departmental Appeals Board responsibility for adjudicating civil money penalties[5] and exclusions[6] imposed under a wide range of fraud and abuse authorities.
- 1993: The Secretary, HHS, delegated to the Departmental Appeals Board responsibility for hearing appeals in provider and supplier participation, enrollment and enforcement cases brought by the Centers for Medicare & Medicaid Service (CMS).[7]
- 1995: After the Social Security Administration (SSA) became an independent agency,[8] the Secretary, HHS, delegated to the Board Chair the Medicare Appeals Council function of hearing appeals in Medicare coverage, payment and entitlement cases.
- 2006: At this time, HHS issued Final Rules which provided for the Departmental Appeals Board to exercise final review authority over disputes involving the imposition of civil money penalties for violation of the Administrative Simplification provisions of Title II of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and its implementing regulations.[9]
Today, the Departmental Appeals Board serves as the final administrative arbiter of a significant number of discrete administrative actions that have been taken by various HHS agency components and have been appealed by the affected individual or entity. Notably, the areas of responsibility listed above are only a small sample of the 60+ statutory and regulatory provisions where the Departmental Appeals Board has been delegated responsibility for resolving administrative disputes. The Board’s primary jurisdictional authorities[10] are set out below:

II. Structure of the Departmental Appeals Board:
Organizationally, the Departmental Appeals Board consists of five separate divisions, each of which are discussed below:
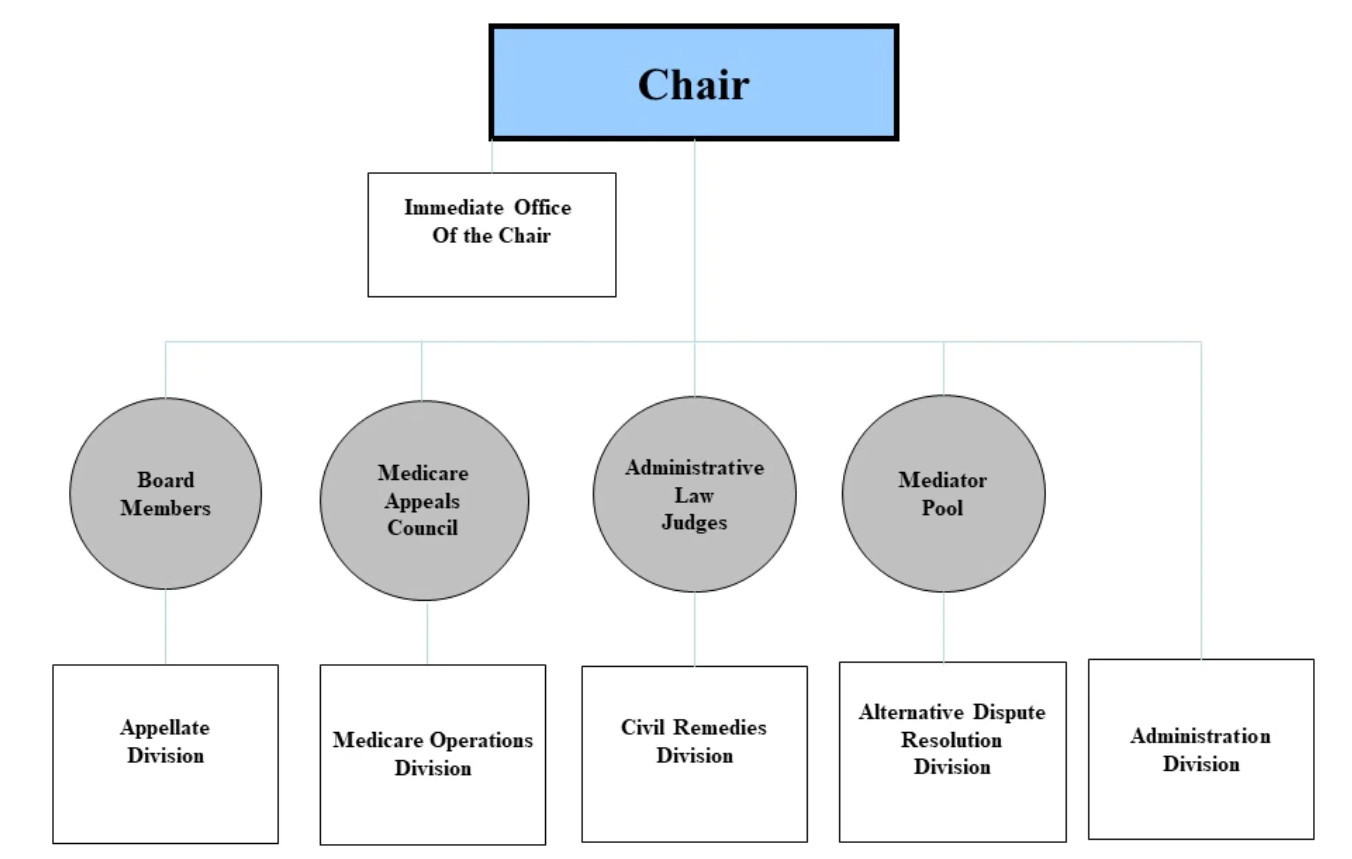
- Appellate Division. The Appellate Division (the Board) is responsible for hearing the appeals of decisions made by Administrative Law Judges in the Civil Remedies Division. It is composed of judges who have been appointed to the Board by the Secretary, HHS. These individuals are career civil servants who typically have extensive experience in the law. Appeals to the Board are reviewed on a de novo basis. In addition to hearing appeals out of the Civil Remedies Division, the Board is also responsible for hearing the appeals of ALJ decisions arising out of a number of other HHS divisions and components. Staff within the Appellate Division provide support for the members of the Board.
- Medicare Operations Division. The Medicare Operations Division provides staff support to the Administrative Law Judges (ALJs) on the Medicare Appeals Council (the Council). The Council provides the final administrative review of claims for entitlement to Medicare and individual claims for Medicare coverage and payment filed by beneficiaries or health care providers/suppliers. The Council is responsible for reviewing ALJ decisions on Medicare payment and coverage matters.
- Civil Remedies Division. The Civil Remedies Division provides legal and administrative support for the Departmental Appeals Board’s Administrative Law Judges (ALJs). The ALJs are qualified under the Federal Administrative Procedure Act to conduct hearings on the record. Generally, the ALJ decision is an initial decision that may be appealed to the Board. If the ALJ decision is not appealed, it is the final administrative decision.
- Alternative Dispute Resolution Division. The Alternative Dispute Resolution Division provides Alternative Dispute Resolution (ADR) services in appeals filed with the Board's other three Divisions (Appellate, Civil Remedies and Medicare Operations Division).
- Administrative Division. The Administrative Division at the HHS Departmental Appeals Board handles a variety of administrative functions for the Board and its staff. These tasks, include, but are not limited to:
- Case Management: The Administrative Division is responsible for managing the flow of cases through the DAB. This includes assigning cases to Administrative Law Judges (ALJs), scheduling hearings, and preparing transcripts.
- Staff support: The Administrative Division provides staff support to the ALJs and the Board Members. This includes providing legal research, drafting orders and decisions, and responding to public inquiries.
- Training: The Administrative Division provides training to ALJs and staff on a variety of topics, including case management, legal research, and writing skills.
- Program Evaluation: The Administrative Division conducts program evaluations to ensure that the DAB is operating efficiently and effectively.
III. What is the Difference Between the Departmental Appeals Board and the Medicare Appeals Council?
Although the Medicare Appeals Council is a component of the Departmental Appeals Board, these entities play very different roles in the administrative appeals process. Part of the confusion that arises is due to the fact that both the Departmental Appeals Board and the Medicare Appeals Council are responsible for serving as the final administrative arbiter of decisions issued by lower-level Administrative Law Judges. The differences between these entities are essentially jurisdictional. For example:
- Departmental Appeals Board: Disputes heard by the Departmental Appeals Board include but are not limited to appeals of ALJ decisions issued in exclusion actions, provider enrollment actions, civil monetary penalty impositions and other enforcement actions taken against nursing home providers, clinical laboratories, home health agencies and other health care providers. Reviews by the Departmental Appeals Board are conducted on a de novo basis.
- Medicare Appeals Council: The Medicare Appeals Council (the Council) falls under the Departmental Appeals Board but is specifically focused on appeals of ALJ decisions in Medicare-related administrative payment and coverage appeals. The Council acts as the final level of administrative review of payment and coverage appeals within HHS. If a party is dissatisfied with an ALJ's decision, the dissatisfied party can request a review by the Medicare Appeals Council. The Council also has the authority to review a decision even if the provider has prevailed and has not filed an appeal. Upon review, the Council evaluates the ALJ's decision and may either uphold, modify, reverse, or remand the decision back to the ALJ for further review and action.
IV. Appeal Requirements Vary by Type of Appeal:
As previously discussed, the Departmental Appeals Board handles disputes handled by ALJs hearing matters falling under the 60+ statutory and regulatory provisions where the Board has been delegated responsibility for resolving certain administrative disputes arising out of various HHS agencies and offices. Due to the extensive scope and variety of administrative appeals involved, we don’t recommend that you assume that the same deadlines and rules for filing an appeal to the Board are the same under each program. Several of the more common appeals falling under the jurisdiction of the Departmental Appeals Board are exclusion and provider enrollment actions. The basic rules to file each of the appeals are discussed in the section below.
V. Case Example -- Challenging an Administrative Exclusion Imposed by the OIG:
Among its many provisions, the “Medicare-Medicaid Anti-Fraud and Abuse Amendments”[11] mandated the exclusion of physicians and other practitioners convicted of program-related crimes from participation in Medicare and Medicaid.[12] The authority to administratively exclude an individual or entity from participating in Federal health benefits programs was first delegated by the Secretary, HHS to the OIG in 1988.[13]
OIG exclusion actions fall into two categories – Mandatory and Permissive. Mandatory actions are required by law to be imposed if the conduct at issue falls into one of the mandatory exclusion categories covered by statute.[14] 42 U.S.C. § 1320a-7(a)(1)-(4). Unlike mandatory exclusion actions, permissive exclusion actions[15] are discretionary – at the option of the OIG.[16] With minor exceptions, the process for appealing a proposed exclusion action is the same, regardless of whether the basis for exclusion is mandatory or permissive. An overview of the steps taken in the appeal of an exclusion is set out below:
- Appeal Level #1: Initially Responding to an Exclusion Action. When seeking to impose an exclusion action, the OIG will likely take one of two approaches when first contacting the affected individual or entity. If the basis for exclusion is mandatory in nature, the OIG will likely send a “Notice of Exclusion” to the affected party. The Notice of Exclusion letter will include information regarding a party’s right to appeal. Nevertheless, the exclusion action will be effective 20 days after the date of the Notice of Exclusion. In contrast, if the basis for exclusion is one of the many permissive bases that has been authorized, the OIG will typically send out a letter titled “Notice of Intent to Exclude” to the affected party. Should the affected party desire to respond to the proposed exclusion action, any arguments, evidence and other mitigating factors must be submitted within 30 days in order for the information to be considered by the OIG as part of its decision-making process.[17] To the extent that an affected party has submitted information to be considered by the OIG, the arguments and evidence will be reviewed prior to deciding whether to impose the contemplated exclusion, modify the exclusion action that has been proposed OR dismiss the exclusion action.
- Appeal Level #2: Appeal of the OIG’s Decision to an ALJ. Should the OIG choose to move forward with an exclusion action, an excluded party has the right to request a formal hearing before an ALJ within 60 days of the date of the OIG’s decision letter. When requesting an ALJ hearing on the matter, the excluded party must submit a written request. The request must set out the reasons why the exclusion action should not be imposed.[18] The ALJ will conduct a formal hearing where you can present evidence, call witnesses, and make legal arguments to contest the exclusion. The ALJ will issue a written decision based on the evidence and arguments presented.
- Appeal Level #3: Appeal to the Departmental Appeals Board. If either party is dissatisfied with the ALJ's decision, they can appeal to the Departmental Appeals Board (DAB) within 30 days of the date of service of the ALJ decision.[19] The DAB will review the ALJ's decision, along with any additional written arguments and evidence submitted by the parties. The DAB can affirm, modify, or reverse the ALJ's decision. Their decision will be in writing and will constitute the final agency action.
- Appeal Level #4: Filing for Judicial Review. If you are still dissatisfied with the outcome, you have the option to seek judicial review in federal court. You must file a lawsuit within the appropriate timeframe and follow the court's procedures for review. An affected individual or entity that is dissatisfied with the Board's decision and is entitled to judicial review must commence civil action within 60 days after the Board serves the parties with a copy of the decision.
Importantly, the steps outlined above are not intended to be all-inclusive. There are a number of arguments that may be asserted in the defense of a proposed exclusion action. Additionally, to the extent that an exclusion is taken, an affected party may be able to argue that the period of exclusion to be imposed does not exceed the statutory minimum period. We strongly recommend that if the OIG has notified you that it intends to impose an exclusion action, you should engage experienced legal counsel to represent your interests throughout this process.
VI. Case Example -- Challenging a Provider Revocation Action Imposed by CMS:
Under Section 936 of “Medicare Prescription Drug, Improvement and Modernization Act of 2003” [20], the Secretary, HHS was authorized to establish a process for the enrollment in the Medicare program of providers of services and suppliers. In recent years, a number of changes have been made to address program integrity concerns in the provider enrollment process. In September 2019, CMS published a Final Rule titled the “Medicare, Medicaid, and Children's Health Insurance Programs; Program Integrity Enhancements to the Provider Enrollment Process.” [21] The Final Rule under 42 C.F.R. §424.535(a), was published in order to implement sections 1866(j)(5) and 1902(kk)(3) of the Social Security Act (as amended by the Affordable Care Act). As a review of the document will show, the Final Rule implemented a wide range of new enrollment, affiliation, revocation and denial authorities. Under the Final Rule, the number of regulatory bases upon which revocation can be based has now grown to 22. In addition to greatly expanding the reasons that can be cited by CMS when revoking a health care provider’s enrollment and participation in the Medicare program, the Final Rule also extended the period that a provider can be barred from reenrolling the Medicare program from three years to a maximum of ten years.[22] Today, Medicare revocations actions are regularly pursued by CMS. When this occurs, the appeals process is as follows:
Generally, the Medicare revocation appeals process is set out under 45 C.F.R. §405.803, “Appeal Rights”. As this provision outlines, a provider is entitled to challenge the revocation of its Medicare billing privileges and may appeal an initial determination made by CMS or its contractor by following the procedures specified in 45 C.F.R. §498. An overview of these provisions is outlined below:
- Preliminary Appeal Determination: Can We File a Corrective Action Plan (CAP)? In limited circumstances, if a provider’s Medicare billing number has been revoked, it may be afforded an opportunity by CMS to take remedial action to correct the deficiencies that were the basis for the revocation action. After the effectuation of the December 2014 Final Rule, only provider’s whose Medicare billing privileges have been revoked due to non-compliance under 42 C.F.R. §424.535(a)(1) are entitled to submit a CAP. The other regulatory bases for revocation are not eligible for CAP remediation. To the extent that your revocation action falls within category, the CAP must be submitted within 30 days of the date of the revocation notice and must provide evidence that the provider is now in full compliance with its applicable obligations. If the provider can demonstrate compliance, CMS will reinstate the provider’s billing privileges. If the CAP is denied, the provider can still exercise its appeal rights under Part 498. Importantly, the submission of a CAP does not “stay” your appeal deadlines. More than likely, you will therefore pursue a dual-track approach is challenging the revocation action.
- Appeal Level #1: Reconsideration. The first level of appeal for a provider to contest the revocation of its Medicare billing privileges is known as the “Reconsideration” level. A reconsideration request must be submitted within 60 days from receipt of the notice of initial determination. Take care, some appeals will be filed with the CMS Provider Enrollment Operations Group (PEOG) while others must be filed with the Medicare Administrative Contractor (MAC). Any documentary evidence a provider wants considered by the hearing officer assigned to their case must be submitted at this level of appeal. If a provider later wants to submit documentary evidence into the record, an Administrative Law Judge (ALJ) will require that the provider show “Good Cause” exists for the late submission of the evidence. “Good Cause” is rarely found to exist absent evidence of an Act of God that prevented earlier submission.
- Appeal Level #2: Administrative Law Judge (ALJ) Hearing. Should you not prevail at the reconsideration level of appeal, you can seek a hearing before an ALJ of the HHS Departmental Appeals Board, Civil Remedies Division. Requests for an ALJ hearing must be submitted within 60 days from the date of the reconsideration decision. The ALJ hearing is like a “mini-trial”. The government will be represented by an attorney assigned by your HHS Regional Office of General Counsel. If the facts in the case are contested, both sides will typically submit briefs, introduce evidence and present witness and / or expert testimony. If both sides agree as to the basic facts in the case, the ALJ will often issue his / her ruling based on the written record.
- Appeal Level #3: Departmental Appeals Board (DAB) Hearing. Both the provider and CMS may contest a decision of the ALJ. Should a party choose to do so, they must request review of the ALJ’s decision by the Departmental Appeals Board, Appellate Division within 60 days of the date of the ALJ’s decision. Importantly, this is the end of the proverbial line administratively. If a provider is dissatisfied with the DAB’s ruling, it must seek judicial review.
- Appeal Level #4: Judicial Review. If a provider wishes to challenge the decision of the DAB, it must file a civil action in U.S. District Court within 60 days of the date of the DAB decision. If a provider can show “Good Cause,” the DAB is permitted to extend the civil action filing deadline.
VII. Case Example -- Challenging the Imposition of Penalties Based on Violations of the HIPAA Administrative Simplification Provisions:
Under the Health Information Portability and Accountability Act of 1996 (HIPAA), the Secretary, HHS, is authorized to impose civil monetary penalties on covered entities and business associates that violate HIPAA’s administrative simplification provisions. In 2000, the Secretary, HHS, delegated this authority to the Director, Office for Civil Rights (OCR).[23] More often than not, the relevant requirements that have not been met are associated with a covered entity’s failure to comply with HIPAA’s “Security Standards for Health Information – Safeguards” [24] which requires that covered entities who maintain or transmit health information:
As a general rule, the Secretary, HHS (through the Director, OCR) may impose a civil money penalty on a covered entity or business associate if it is determined that the entity has violated an administrative simplification provision.[25] If such a penalty has been proposed, the initiation of the case and the appeals process followed includes the following:
- Investigation by OCR Staff. Upon receipt of a complaint, breach report, or proactive compliance review, OCR will typically determine whether there is sufficient information to open a file and conduct an investigation of the allegations to determine whether an actionable violation of the HIPAA administrative simplification rules has occurred.
- Appeal Level 1: Findings and Opportunity to Respond. After completing the investigation, the OCR will provide the covered entity with written findings and give them an opportunity to respond. The covered entity can submit written evidence, legal arguments, or other relevant information to dispute the findings. Before imposing civil money penalties, the OCR may offer the covered entity an opportunity for informal resolution. This can involve negotiation, settlement discussions, or the development of a corrective action plan.
- OCR Issues a “Notice of Proposed Determination” to the Affected Entity. Based on the investigation and the covered entity's response, the OCR will make a determination regarding whether a violation has occurred. If a violation is found, the OCR will issue a “Notice of Proposed Determination” which outlines the alleged violations and the statutory basis for any proposed penalties. The notice will also include “Findings of Fact” upon which the OCR has made it proposed determination. Finally, the notice will include a summary of the entity’s appeal rights and the procedures which must be followed when requesting a hearing before an Administrative Law Judge.
- Appeal Level #2: Filing for Hearing Before an Administrative Law Judge. If the affected entity requests a hearing, an administrative law judge will review the case. The administrative hearing provides an opportunity for the covered entity to present evidence, cross-examine witnesses, and argue its case. The Administrative Law Judge will issue a recommended decision to the OCR.[26]
- Appeal Level #3: Requesting Review by the Departmental Appeals Board. Any party may appeal the decision of the ALJ to the Departmental Appeals Board by filing a notice of appeal with the DAB within 30 days of the date of service of the ALJ decision.[27] The decision of the Board (other than a remand by the Board to the ALJ) becomes the final decision of the Secretary 60 days after the date of service of the Board’s decision unless a party files a motion for reconsideration with the Board in accordance with 45 C.F.R. § 160.548(j).
- Appeal Level #4: Judicial Review. An affected entity must file any petition for judicial review within 60 days of the date on which the decision of the Departmental Appeals Board becomes the final decision of the Secretary.[28]
VIII. Conclusion:
As reflected above, the appeals procedures leading up to a review by the Departmental Appeals Board vary widely from program to program. When appealing these cases, experience counts. Individuals and entities appealing an administrative matter before the HHS Departmental Appeals Board should strongly consider being represented by experienced health law counsel for several reasons. First and foremost, experienced legal counsel will bring a level of expertise and knowledge of the complex legal and regulatory framework surrounding this complex appeals process. They will be familiar with the specific laws, regulations, and precedents relevant to this specific type of case. Second, experienced legal counsel can assist you in navigating the administrative procedures effectively. They can help ensure that all necessary documentation is submitted within the required timelines and that applicable procedural requirements have been followed. Additionally, experienced legal counsel can provide objective guidance, ensuring that an appellant’s rights and interests are protected throughout the appeals process. Overall, experienced legal counsel provides invaluable support, knowledge, and advocacy for individuals appealing a matter before the HHS Departmental Appeals Board. Liles Parker attorneys have extensive knowledge of the appeals process and experience in handling complex health law matters. Give us a call for a free consultation on your case. 1 (800) 475-1906.

Robert W. Liles, J.D. is an experienced health lawyer and a former Federal prosecutor. Robert and the other attorneys at Liles Parker represent healthcare providers and suppliers around the country in HHS administrative appeals. Should your practice or clinic be subjected to a revocation or another action that is appealed to the Departmental Appeals Boards, give us a call for a free consultation. We can be reached at: 1 (800) 475-1906.
- [1] HHS webpage. https://www.hhs.gov/careers/working-hhs/agencies#:~:text=HHS%20employs%20more%20than%2080%2C000,States%20and%20 around%20the%20world .
- [2] See https://www.hhs.gov/about/agencies/orgchart/index.html.
- [3] As set out in the “Background” section of the Departmental Appeals Board website, the Board is responsible for reviewing disputed decisions in a wide range of HHS-related programs, involving more than 60 statutory provisions.
- [4] https://grants.nih.gov/grants/guide/historical/1973_05_29_Vol_02_No_02.pdf Notice of proposed rulemaking was published in the Federal Register on November 18, 1972, at 37 Fa 24675, setting forth a charter for a Departmental Grant Appeals Board from which grant appeals panels would be selected for the purpose of reviewing and providing hearings upon post-award disputes which may arise in the administration of certain grant programs by constituent agencies of the Department of Health, Education, and Welfare (HEW).
- [5] Civil money penalties imposed by the OIG can be challenged by individuals and entities through the administrative appeals process. 20 C.F.R. §498.103. Once appealed to an ALJ (20 C.F.R. §498.202), if not satisfied with the decision, an appellant may advance the case to be heard by the Departmental Appeals Board. 20 C.F.R. §498.221.
- [6] The OIG is authorized to propose to exclude individuals and entities from participation in Federal health benefit programs. 42 C.F.R. §1001.1(a) and (b). A request for a hearing by an ALJ must be made in writing and must set out the specific issues or findings of fact and conclusions of law with which the respondent disagrees. 42 C.F.R. §1005.2(d). If the respondent is dissatisfied with the initial decision of the ALJ, the respondent may file a notice of appeal with the DAB within 30 days of the date of service of the initial ALJ decision. 42 C.F.R. §1005.21(a).
- [7] At this time, CMS was known as the Health Care Financing Administration (HCFA). The name was changed to the Centers for Medicare & Medicaid Services on June 14, 2001.
- [8] 61 FR 32347 (June 24, 1996).
- [9] 71 FR 8389 (February 16, 2006).
- [10] A copy of this chart can be found on HHS’s website.
- [11] Public Law 95-142.
- [12] Now codified at Section 1128 of the Social Security Act.
- [13] The authority to exclude was granted to the Secretary, HHS in the Civil Money Penalties Law (Public Law 97-35, 1981 (as codified at section 1128A of the SSA). The Secretary delegated it to its Office of Inspector General in 1988 (53 Fed. Reg. 12,993 (April 20, 1988)).
- [14] 42 U.S.C. §1320a-7(a)(1)-(4).
- [15] 42 U.S.C. §1128(b)(1)-(b)(16) and §1156 of the Social Security Act.
- [16] For a more detailed discussion of Medicare exclusion risks, see our article titled “Medicare Exclusion Risks: Employing Excluded Individuals Can Result in Significant Administrative, Civil and / or Criminal Liabilities.”
- [17] It is worth noting that recent letters to individuals and entities proposing to impose an exclusion action have not been titled either “Notice of Exclusion” or “Notice of Intent to Exclude.”
- [18] See 42 C.F.R. §402.19, 1001.2007, 1003.109(b), and 1004.140(b).
- [19] See 42 C.F.R. §1005.21(a).
- [20] This legislation amended Section 1866 (j) of the Social Security Act.
- [21] 84 FR 47794 (September 10, 2019).
- [22] For additional information on the various bases that can cited when revoking a provider’s enrollment in the Medicare program, see our article titled “Home Health Revocation Actions by Medicare are Expanding Around the Country.”
- [23] 65 FR 82381 (December 28, 2000).
- [24] 42 U.S.C. § 1320d-1(d)(2)
- [25] 45 C.F.R. §160.402.
- [26] 45 C.F.R. §160.402(b).
- [27] 45 C.F.R. §160.548(a).
- [28] 45 C.F.R. §160.548(k)(1).
