(March 26, 2010): Over the next few days, we will be publishing a brief overview of specific Zone Program Integrity Contractors (ZPICs) (such as AdvanceMed) – the companies who have been hired by CMS to conduct the medical reviews of Part A and Part B health care providers around the country. As we have previously discussed, over the last year, ZPICs have been taking over where Program Safeguard Contractors (PSCs) left off. While our firm is still handling a number of cases that were initiated by PSCs, all of our recent cases have involved ZPICs. As ZPICs have been so quick to point out, they are not paid a percentage of the Medicare overpayments identified like their fellow medical reviewers – Recovery Audit Contractors (RACs). Nevertheless, as you will soon see, they are handsomely paid for their efforts, albeit in a different fashion than are RACs. It is essential to keep in mind that ZPICs are designed to "find and prevent waste, fraud and abuse in Medicare."Further, like their RAC cousins, ZPICs look at billing trends and patterns, focusing on providers whose billings for Medicare services are higher than the majority of providers in the community (e.g. their peers).
I. Where is AdvanceMed Currently Operating?
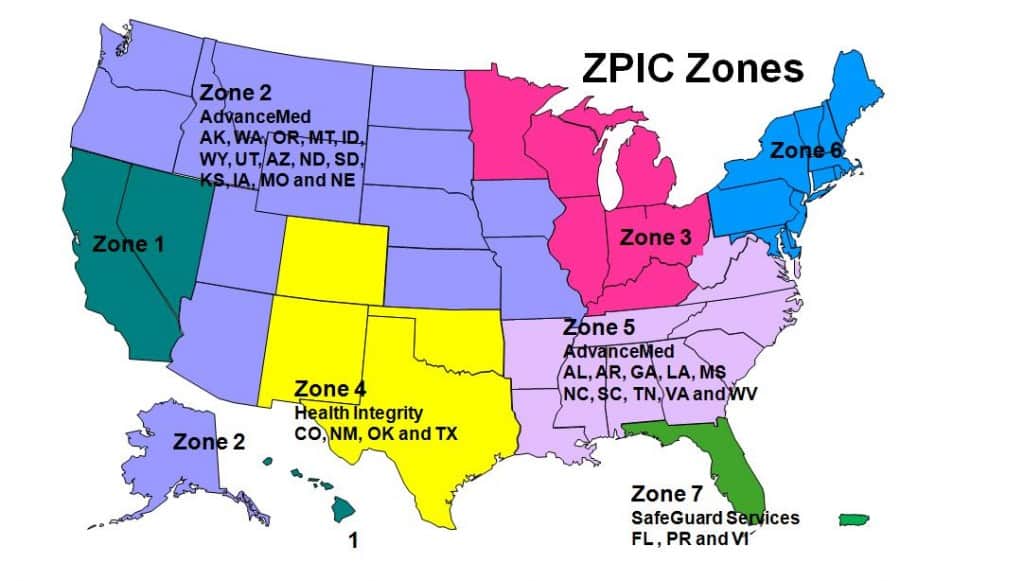
Initially, AdvanceMed Corporation was awarded a $107,957,737.00 five-year contract to handle the ZPIC duties for Zone 5. Zone 5 covers the states of Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia. Yes, you read this correctly, AdvanceMed is being paid over $100 million for just one contract.
As the ZPIC for Zone 5, AdvanceMed assumed the Benefit Integrity functions for Medicare Parts A, B, Durable Medical Equipment, and Home Health and Hospice, as well as establishing a Medicare / Medicaid (Medi-Medi) data matching program for each state within the Zone. The AdvanceMed Zone 5 ZPIC contract performs the following functions for CMS as a ZPIC:
- Medicare fraud investigation and prevention, including referrals to law enforcement;
- Medicare data analysis (discovery, detection, investigation, and overpayment projection);
- Medical Review to support fraud case development, including coverage and coding determinations;
- Reviewing audit, settlement, and reimbursement of cost reports, and conducting specified audits;
- IT Systems for case and decision tracking and data warehousing;
- Interface with the Medicare contractors, the medical community (outreach & education), and law enforcement; and
- Medicare/Medicaid data matching program safeguards work for each state in Zone 5.
II. Many AdvanceMed Audits Will Involve the Extrapolation of Alleged Damages:
Over the years, we have gone up against AdvanceMed numerous times, challenging their interpretation of LMRPs / LCDs and assessing the methods they utilized to engage in a statistical extrapolation of the alleged damages in our client’s cases. To give the company its due – their statistical experts are smart, aggressive and do not hesitate to respond when their methods have been challenged. We like that – it keeps us sharp.
With the help of some of the best statisticians in the country (including, but not limited to the late Will Yancey, Ph.D.), in a number of cases, we have been able to show that their extrapolation of damages (and that of other ZPICs) has not complied with applicable requirements, and is therefore invalid. To be fair, every extrapolation is different, both in terms of facts, the methodology employed, and in the associated calculations conducted. As attorneys, we work with our experts to break down and assess AdvanceMed’s (and other ZPICs) calculations. Perhaps they handled it appropriately – or maybe they didn’t. There really isn’t any way to know if it was handled properly without a complete copy of their file (including associated work papers and calculations) so that we can fully assess their actions.
Over the last year, we have seen a marked increase in contractor (ZPIC) participation (as "participants" not as "parties") in ALJ hearings. Their experts have consistently been professional, concise and ready to answer any questions posed by the ALJ. Our recommendation – both counsel and their defense expert better be prepared. It's never to early to start thinking about how to best contest the extrapolation that has been conducted. As a final point, we are aware of a number of instances where a provider (or their representative) has chosen to ignore the extrapolation as a contestable issue. In other words, they just accept the extrapolation as a foregone conclusion and focus solely on the claims. We disagree with that approach. If we identify deficiencies with the extrapolation, we aggressively challenge its application.
III. AdvanceMed Medical Reviews Need to be Carefully Assessed:
Once a provider has been identified as an outlier (or identified as a possible problem through a variety of other mechanisms), a medical review of their claims is often conducted by a ZPIC, such as AdvanceMed.
A number of year ago, Kevin Gerold, CMS’ former Acting Deputy Director for Program Integrity was quoted as saying that the agency had revamped its approach to claims processing in an effort to better “grasp the experience of the patient encounter.” Mr. Gerold was further quoted as saying that CMS was going to “let medical reviewers assess a claim’s legitimacy based on the big picture of the patient encounter, not on a nit-picking slavery to perfect documentation.” Unfortunately, in our opinion, AdvanceMed’s medical reviews have been extremely technical -- resulting in the denial of many claims based on minor omissions, technical deficiencies and / or the contractors’ own peculiar spin regarding the application of an LCD.
In responding to AdvanceMed’s reasons for denial, it is essential that you obtain each and every reference relied upon by the contractor when denying the claims at issue. We have identified multiple instances where a Medicare contractor (not necessarily AdvanceMed) attempted to apply an LCD retroactively. Moreover, it is important to examine the underlying statutory authority to determine whether the contractor’s interpretation of a coverage provision is consistent with the underlying law or regulation. Finally, it isn’t enough to merely “poke holes” in AdvanceMed’s reasons for denial. Specifically show that the particular claims at issue do, in fact, qualify for coverage and payment.
IV. Conclusion:
The bottom line is simple -- if you are audited by AdvanceMed, your Medicare claims will be scrutinized like never before. While we often disagree with AdvanceMed's findings, we have consistently found them to be professional in their dealings and consistent in their arguments. Regardless of whether or not you ultimately choose to be represented by our law firm, we strongly recommend that you seek legal representation if your practice or clinic is audited by AdvanceMed.

Our attorneys have years of experience representing Medicare providers in connection with post-payment audits and other administrative actions taken by UPICs, ZPICs and other Medicare contractors. Should you have any questions regarding these issues, don’t hesitate to contact us. For a complimentary consultation, you may call Robert W. Liles or one of our other attorneys at 1 (800) 475-1906.

You must be logged in to post a comment.